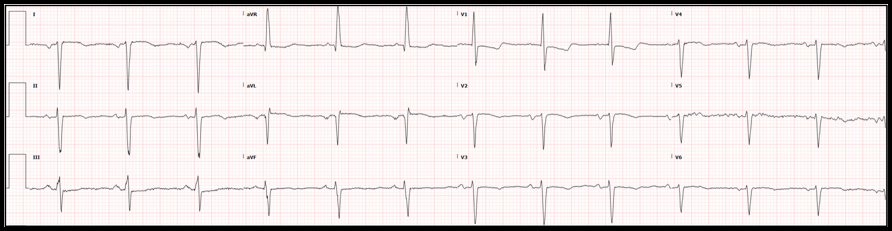
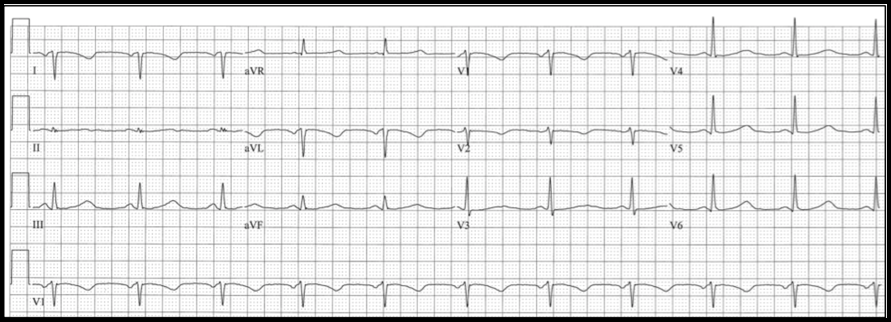
By: Andrew Yde, MD Editors: Drs. Littmann and Gibbs Case: A 61-year old woman with coronary artery disease and interstitial lung disease, on home O2 therapy, presented with a 3-day history of constant right-sided chest pain radiating to the right neck. She also complained of worsening dyspnea and exertional lightheadedness. On physical examination, the patient was afebrile, had a heart rate in the 60s, was mildly hypertensive at 147/71 mmHg, and was maintaining normal oxygen saturations on 2L supplemental O2. The examiner did not note abnormalities on cardiopulmonary exam. Chest CT angiogram was negative for pulmonary embolism and high sensitivity troponin was <6. She was given morphine and Toradol with some relief in her chest pain. The following electrocardiogram was obtained: Physician interpretation of the ECG was as follows: Normal sinus rhythm with a rate of 67, right axis deviation, otherwise normal intervals. ST depression in the septal and lateral leads. No ST elevation. When compared to an ECG obtained two months before, the complex morphology is generally unchanged. The ST depression is a bit more pronounced. What is your interpretation of this initial ECG? Do you agree with the physician interpretation?
Do not agree. The ECG shows sinus rhythm with dextrocardia. The ST-T morphology cannot be reliably assessed. Repeat ECG with limb leads reversed, and place right-sided chest leads. Summary of key ECG findings:
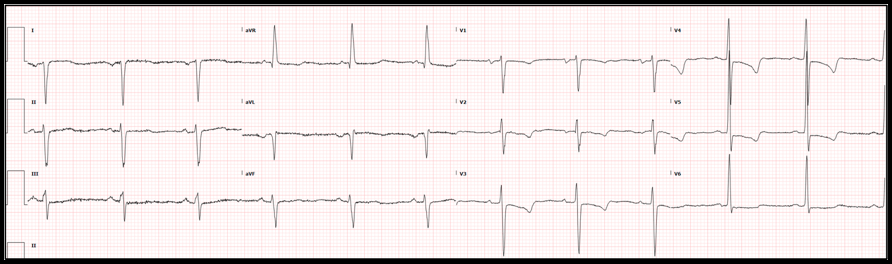
In this patient with dextrocardia, the chest leads were reversed but the limb leads were not. See ECG below:
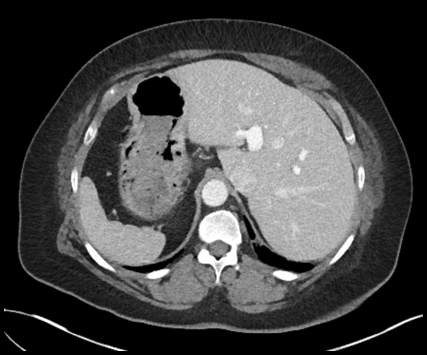
Note that the limb leads remained unchanged, but the QRS progression in the chest leads has normalized. One can now diagnose probable left ventricular hypertrophy (LVH) with secondary repolarization abnormality vs. anterolateral ischemia. As the repolarization abnormality was identical to that seen two years before, LVH was the more likely diagnosis. Possible abnormalities in the limb leads may have remained obscure. Proof of situs inversus totalis:
Hospital Course:
Two sets of high-sensitivity troponin measurements remained within normal limits. An echocardiogram showed new moderate biventricular dysfunction with left ventricular ejection fraction (LVEF) calculated at 35%, changed from echocardiogram three years prior in which biventricular function was normal and LVEF was 55%. Given a history that was concerning for ischemia and new biventricular dysfunction, the Cardiology service recommended cardiac catheterization which revealed calcification and minor luminal irregularities of all coronary vessels and a 50% stenosis of the mid left main coronary artery. No stents were placed, and medical management was recommended. The patient experienced several bouts of right sided chest pain reliably relieved by oral Tylenol. Her chest pain was felt to be musculoskeletal in nature. She was discharged in stable condition with follow-up appointments with both her primary care physician and Cardiology. What is situs inversus, and what does it mean for our patient? Situs solitus refers to the normal orientation/location of the thoracic and abdominal viscera. In situs solitus, we find a tri-lobed right lung, a bi-lobed left lung, and a heart on the left side with the apex facing left. The liver and gallbladder are on the right, the spleen is present on the left, the descending colon is on the right, the ascending colon on the left, and the inferior vena cava (IVC) runs to the right of the aorta in the abdomen, etc. In 1 out of 10,000 people, the orientation of the thoracic and abdominal viscera is reversed - a heterotaxy syndrome called situs inversus. Of these patients, the vast majority have situs inversus totalis, in which the heart is in the right chest with the apex oriented toward the right (dextrocardia). The remainder of the thoracic and abdominal viscera are in positions exactly mirroring situs solitus. For example, the right lung is bi-lobed, the left lung is tri-lobed, the liver and gallbladder are on the left side, the spleen is on the right side, the ascending colon is on the left, the descending colon is on the right, the IVC runs to the left of aorta in the abdomen, etc. Approximately 2-5% of these patients will have congenital cardiac anomalies, but the vast majority will be asymptomatic with normal quality of life and life expectancy. Approximately 1 in 22,000 people in the general population will have situs inversus with levocardia, meaning that, although the thoracic and abdominal viscera are in mirror/reverse position from situs solitus as in situs inversus totalis, the heart remains in levocardia (its normal orientation), located in the left chest with the apex oriented toward the left. Nearly 100% of these patients have congenital cardiac anomalies, usually of the cyanotic variety (i.e. transposition of the great vessels). These patients have a severely shortened life expectancy. In fact, only about 5-13% of patients with situs inversus with levocardia survive beyond 5 years of age. Of patients with situs inversus totalis, 17-25% will have Kartagener syndrome characterized by chronic sinusitis, bronchiectasis and situs inversus. This syndrome is a result of dynein protein abnormalities causing impaired mucociliary clearance, known as primary ciliary dyskinesia. Interestingly, only 50% of patients with primary ciliary dyskinesia will have situs inversus, and thus only 50% will meet official criteria for Kartagener syndrome. Based on radiographic, echocardiographic, and ECG evidence proving dextrocardia, CT angiography of the chest confirming a tri-lobed left lung and bi-lobed right lung, and CT abdomen obtained during previous hospital admission, our patient has situs inversus totalis without associated primary ciliary dyskinesia. She had no evidence of congenital cardiac abnormalities on her echocardiogram or catheterization. She had respiratory bronchiolitis associated interstitial lung disease and chronic obstructive pulmonary disease, both secondary to a greater than 25 pack-year history of cigarette smoking, rather than chronic sinusitis. This patient’s coronary disease did not seem to be related to her underlying situs inversus totalis, but rather due to the significant smoking history, diabetes, and hypertension. Dr. Littmann’s comments:
If you order an ECG, please spend a couple of minutes to analyze it. The first steps include rate, regularity and rhythm. Then go left-to-right, starting with the P waves. The normal sinus P wave cannot be negative in lead I as the SA node is in the upper right atrium and therefore, atrial activation is right-to-left, going towards lead I. If the P wave is negative in lead I, follow the steps below:
Below is an example of right arm – left arm lead reversal. Note that the limb leads look essentially identical to what was seen in dextrocardia (everything negative in lead I, upright P, QRS and T in aVR and negative P, QRS and T in aVL), but in the chest leads, there is normal R-wave progression.
References:
0 Comments
Your comment will be posted after it is approved.
Leave a Reply. |
AuthorThis blog represents important ECG lessons that the Emergency Medicine Residents from Carolinas Medical Center (Charlotte, NC) rotating through the Cardiology service encounter. Test your knowledge with them! The esteemed educators Dr. Laszlo Littmann and Dr. Michael Gibbs serve as the primary content editors and course directors. Archives
September 2020
CategoriesAll Bradycardia Cardiology ECG Lesson Heart Block Syncope Ventricular Tachycardia Vtach |
LEGAL DISCLAIMER (to make sure that we are all clear about this):The information on this website and podcasts are the opinions of the authors solely.
For Health Care Practitioners: This website and its associated products are provided only for medical education purposes. Although the editors have made every effort to provide the most up-to-date evidence-based medical information, this writing should not necessarily be considered the standard of care and may not reflect individual practices in other geographic locations.
For the Public: This website and its associated products are not intended to be a substitute for professional medical advice, diagnosis, or treatment. Your physician or other qualified health care provider should be contacted with any questions you may have regarding a medical condition. Do not disregard professional medical advice or delay seeking it based on information from this writing. Relying on information provided in this website and podcast is done at your own risk. In the event of a medical emergency, contact your physician or call 9-1-1 immediately.
For Health Care Practitioners: This website and its associated products are provided only for medical education purposes. Although the editors have made every effort to provide the most up-to-date evidence-based medical information, this writing should not necessarily be considered the standard of care and may not reflect individual practices in other geographic locations.
For the Public: This website and its associated products are not intended to be a substitute for professional medical advice, diagnosis, or treatment. Your physician or other qualified health care provider should be contacted with any questions you may have regarding a medical condition. Do not disregard professional medical advice or delay seeking it based on information from this writing. Relying on information provided in this website and podcast is done at your own risk. In the event of a medical emergency, contact your physician or call 9-1-1 immediately.

 RSS Feed
RSS Feed