|
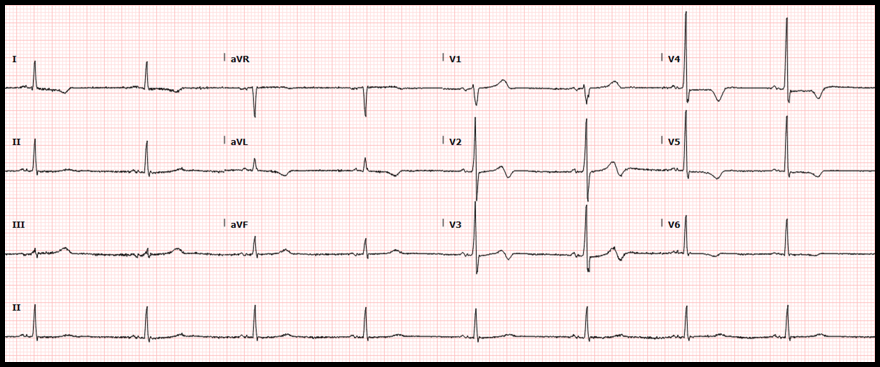
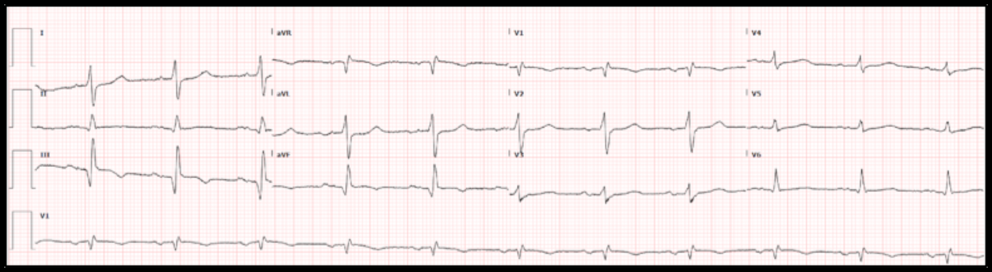
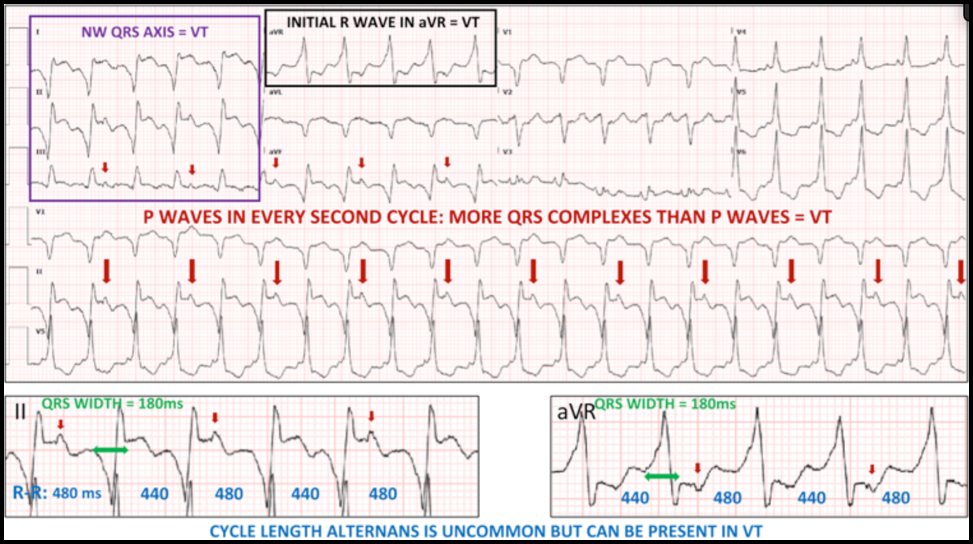
Case: A 69-year old man with ischemic cardiomyopathy (LVEF 30%), and a history of both ventricular tachycardia and recurrent atrial flutter, s/p ICD placement, presented with one day of palpitations and associated lightheadedness. His cardiac medications included amiodarone and apixaban (Eliquis). His heart rate was 131 beats/min and regular, blood pressure was 103/84 mmHg. On exam he was slightly diaphoretic and anxious, but in no acute distress. The ECG interpretation software indicated sinus tachycardia with nonspecific intraventricular conduction delay and acute inferior infarct (LCX). This was over-read by the providers as atypical atrial flutter. He received IV amiodarone bolus and drip. The following electrocardiogram was obtained: Here is the patient’s baseline ECG for comparison: What is your interpretation of the ECGs? Do you agree that this was atrial flutter?
Correct interpretation of the ECG:
Summary of Key Clinical and ECG Findings (see annotated ECG below):
Hospital Course:
The patient remained in WCT overnight. Next morning, he underwent successful electrical cardioversion and was discharged home with a diagnosis of atrial flutter. Over a follow-up of 3 months, he did not have recurrence of the tachycardia. Dr. Littmann’s Comments:
Ventricular tachycardia (VT) is often misdiagnosed as SVT. This phenomenon was first described almost 50 years ago. Despite numerous publications and reviews raising awareness to this problem, the misdiagnosis of WCT, unfortunately, continues to be very common. As described above, there are numerous ECG clues that can help you diagnose VT. The most important factor, however, is the clinical likelihood: of all WCTs, about 80% are VT. In patients with heart disease, 90-95% of WCT is VT. “Probable VT” should always be your default diagnosis. It is OK not to remember any of the ECG clues listed by Drs. Kastner and Plate. If you are not sure, just give IV adenosine. In this case, it is reasonable to raise a few additional legitimate questions: • Why was the VT relatively slow? The patient was on amiodarone which, by suppressing conduction velocity of the reentry circuit, can markedly slow down the rate of VT. • Why did the ICD not shock the patient? Probably because of the relatively slow heart rate. ICDs are usually programmed to deliver shocks at faster rates. • Would it have been important to diagnose, or at least consider, the diagnosis of VT? Yes, because an attempt could have been made to overdrive pace the ventricles with the help of the pacemaker/ICD. Slow VTs are uniquely susceptible to overdrive pacing. If successful, it could have immediately resolved the tachycardia and cardioversion, even hospital admission, may have been avoided. In addition, the ICD could have then been reprogrammed to provide automatic overdrive pacing if a similar tachy-event were to be detected in the future. References:
1. Littmann L, Olson EG, Gibbs MA. Initial evaluation and management of wide-complex tachycardia: a simplified and practical approach. Am J Emerg Med 2019;37:1340-5. 2. Vereckei A, Duray G, Szénási G, Altemose GT, Miller JM. A new algorithm using only lead aVR for the differential diagnosis of wide QRS complex tachycardia. Heart Rhythm 2008;5:89-98.
0 Comments
|
AuthorThis blog represents important ECG lessons that the Emergency Medicine Residents from Carolinas Medical Center (Charlotte, NC) rotating through the Cardiology service encounter. Test your knowledge with them! The esteemed educators Dr. Laszlo Littmann and Dr. Michael Gibbs serve as the primary content editors and course directors. Archives
September 2020
CategoriesAll Bradycardia Cardiology ECG Lesson Heart Block Syncope Ventricular Tachycardia Vtach |
LEGAL DISCLAIMER (to make sure that we are all clear about this):The information on this website and podcasts are the opinions of the authors solely.
For Health Care Practitioners: This website and its associated products are provided only for medical education purposes. Although the editors have made every effort to provide the most up-to-date evidence-based medical information, this writing should not necessarily be considered the standard of care and may not reflect individual practices in other geographic locations.
For the Public: This website and its associated products are not intended to be a substitute for professional medical advice, diagnosis, or treatment. Your physician or other qualified health care provider should be contacted with any questions you may have regarding a medical condition. Do not disregard professional medical advice or delay seeking it based on information from this writing. Relying on information provided in this website and podcast is done at your own risk. In the event of a medical emergency, contact your physician or call 9-1-1 immediately.
For Health Care Practitioners: This website and its associated products are provided only for medical education purposes. Although the editors have made every effort to provide the most up-to-date evidence-based medical information, this writing should not necessarily be considered the standard of care and may not reflect individual practices in other geographic locations.
For the Public: This website and its associated products are not intended to be a substitute for professional medical advice, diagnosis, or treatment. Your physician or other qualified health care provider should be contacted with any questions you may have regarding a medical condition. Do not disregard professional medical advice or delay seeking it based on information from this writing. Relying on information provided in this website and podcast is done at your own risk. In the event of a medical emergency, contact your physician or call 9-1-1 immediately.

 RSS Feed
RSS Feed