|
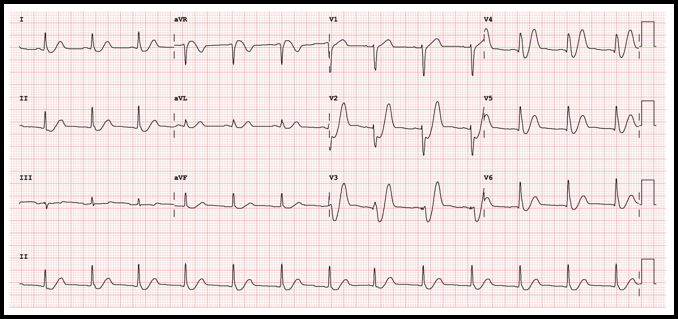
Case: A 36-yo obese female with no other known past medical condition presented to the emergency department with a 30-minute history of chest pain. The pain was described as being a retrosternal pressure-like discomfort that was non-radiating, and 10/10 in severity. The patient denied having similar episodes in the past. There were no alleviating or worsening factors. During the physical examination, the patient was noted to have the Levine’s sign (clenched fist held over her chest). The following electrocardiogram was obtained: ECG Interpretation
Rate: 78/min Rhythm: Normal sinus rhythm Axis: Normal QRS axis QRS: <120 msec; no abnormal Q waves ST-T: ST depression at the J point (at the junction between the QRS complexes and ST segments) in the anterior/lateral leads, mostly upsloping ST segments and then, very tall peaked T waves (de Winter T waves). ST segment elevation in aVR. Significance of ECG Finding
Disposition
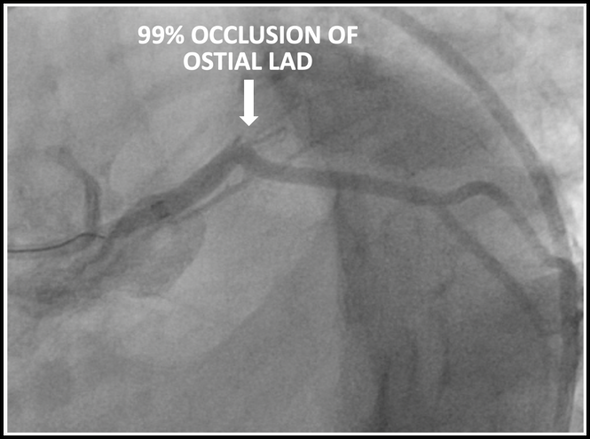
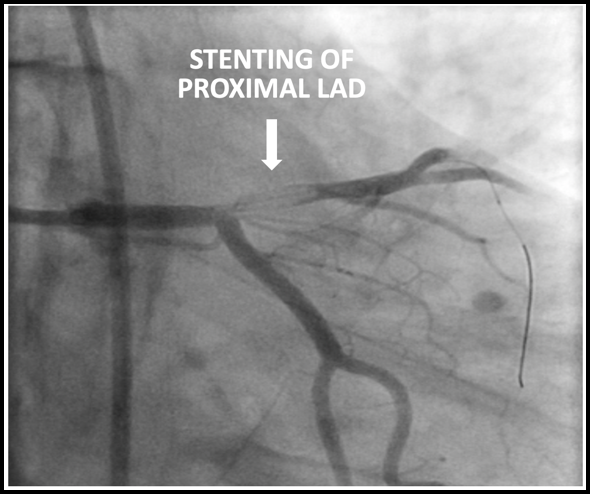
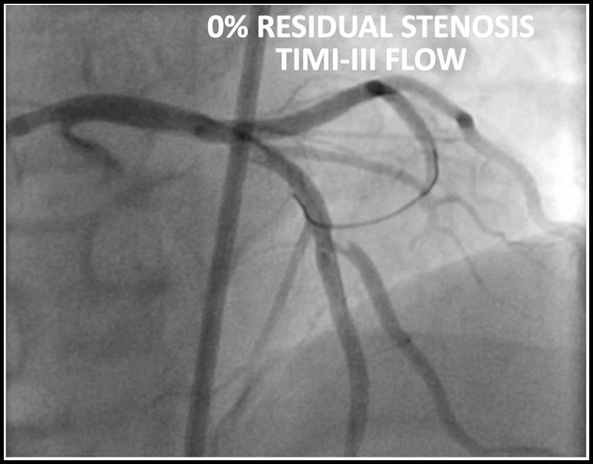
The patient underwent emergent cardiac catheterization which found a 99% occlusion of the ostial LAD. The initial troponin-T was 4.78ng/mL and peaked at >50ng/mL (detection limit) later that day. It is important to remember that a positive troponin is not needed to make the diagnosis of STEMI or a STEMI equivalent.
Results of cardiac catheterization and stenting of the proximal LAD are shown below
Dr. Littmann’s comments:
Drs. Sabatini-Regueria and Fleming have beautifully summarized our current understanding of the de Winter sign, its prevalence, clinical significance, possible mechanism and the somewhat controversial guideline recommendations how to proceed when it is manifest. I have a few comments about the de Winter sign:
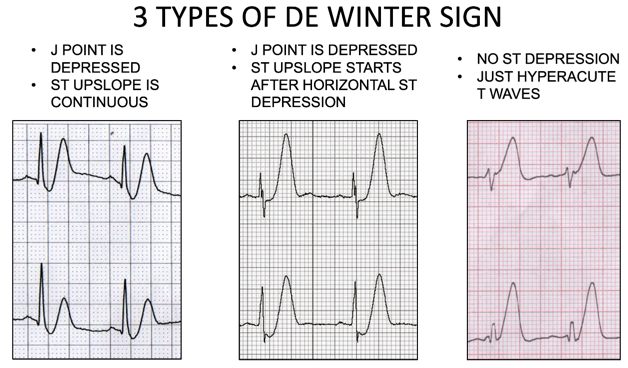
Below are the three types of de Winter ECGs. Note that in the third type, there is no ST depression, just hyperacute T waves.
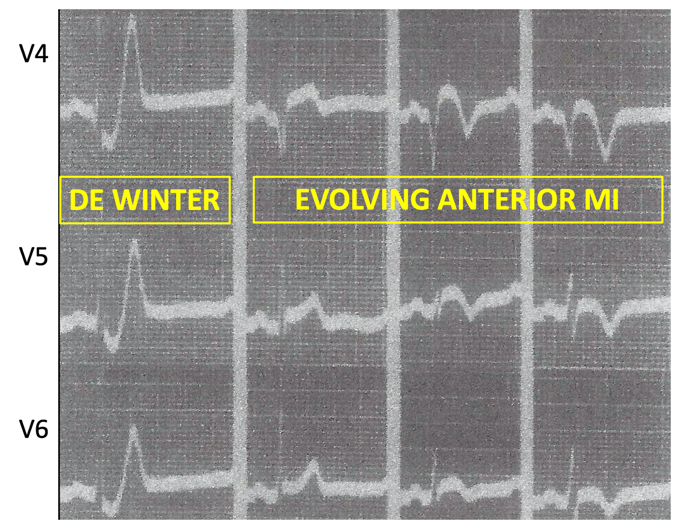
Below is an edited version of the de Winter sign as described by Dr. Dressler in 1947
References (all represented by DOI numbers):
10.1056/NEJMc0804737 10.1016/0002-8703(47)90343-8 10.1016/j.jacc.2018.08.1038 10.1016/j.ajem.2013.09.037 10.12998/wjcc.v7.i20.3296 10.4103/HEARTVIEWS.HEARTVIEWS_90_19 10.1155/2018/6868204 10.21037/atm.2019.07.19 10.1016/j.jelectrocard.2017.08.024 10.1016/j.jacc.2020.07.015
0 Comments
|
AuthorThis blog represents important ECG lessons that the Emergency Medicine Residents from Carolinas Medical Center (Charlotte, NC) rotating through the Cardiology service encounter. Test your knowledge with them! The esteemed educators Dr. Laszlo Littmann and Dr. Michael Gibbs serve as the primary content editors and course directors. Archives
September 2020
CategoriesAll Bradycardia Cardiology ECG Lesson Heart Block Syncope Ventricular Tachycardia Vtach |
LEGAL DISCLAIMER (to make sure that we are all clear about this):The information on this website and podcasts are the opinions of the authors solely.
For Health Care Practitioners: This website and its associated products are provided only for medical education purposes. Although the editors have made every effort to provide the most up-to-date evidence-based medical information, this writing should not necessarily be considered the standard of care and may not reflect individual practices in other geographic locations.
For the Public: This website and its associated products are not intended to be a substitute for professional medical advice, diagnosis, or treatment. Your physician or other qualified health care provider should be contacted with any questions you may have regarding a medical condition. Do not disregard professional medical advice or delay seeking it based on information from this writing. Relying on information provided in this website and podcast is done at your own risk. In the event of a medical emergency, contact your physician or call 9-1-1 immediately.
For Health Care Practitioners: This website and its associated products are provided only for medical education purposes. Although the editors have made every effort to provide the most up-to-date evidence-based medical information, this writing should not necessarily be considered the standard of care and may not reflect individual practices in other geographic locations.
For the Public: This website and its associated products are not intended to be a substitute for professional medical advice, diagnosis, or treatment. Your physician or other qualified health care provider should be contacted with any questions you may have regarding a medical condition. Do not disregard professional medical advice or delay seeking it based on information from this writing. Relying on information provided in this website and podcast is done at your own risk. In the event of a medical emergency, contact your physician or call 9-1-1 immediately.


 RSS Feed
RSS Feed