|
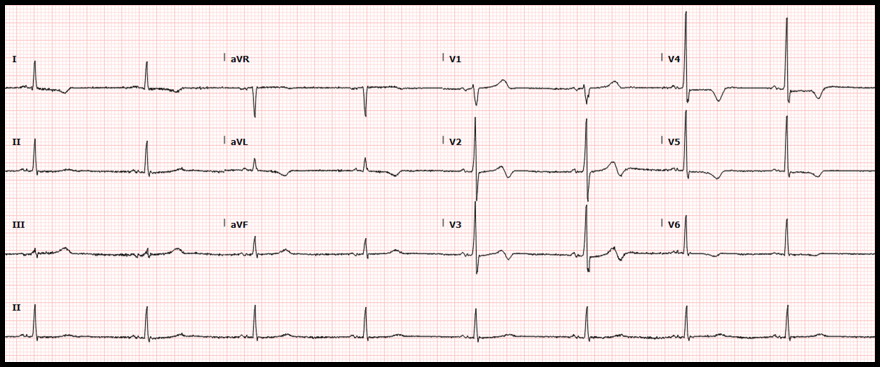
Case: A 56-year-old man with a medical history of schizophrenia, tobacco abuse, and coronary artery disease presented to our emergency department for chest pain. The patient had drug-eluting stents placed to the mid-circumflex and right coronary arteries 13 months before the current presentation. He reports that he has not been taking aspirin or clopidogrel due to financial limitations. He also continues tobacco use of ½ pack a day. The patient describes 3 weeks of severe left-sided, exertional chest pain and associated dyspnea. The pain is normally relieved with rest and ibuprofen, but over the past two days he has had similar pain at rest with only intermittent relief. The following electrocardiogram was obtained: ECG Interpretation:
Diagnosis:
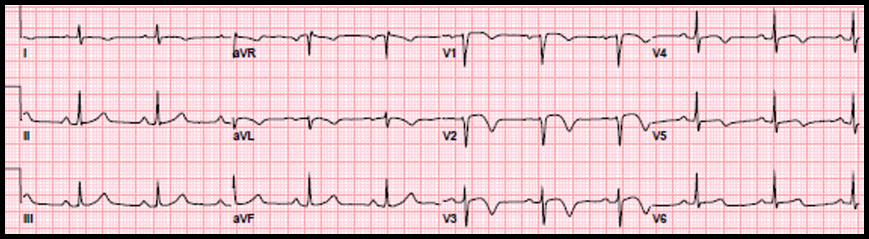
Wellens syndrome Significance of Findings:
Image Source: https://www.ncbi.nlm.nih.gov/books/NBK482490/ Diagnostic criteria of Wellens syndrome:
Management:
Patient Disposition:
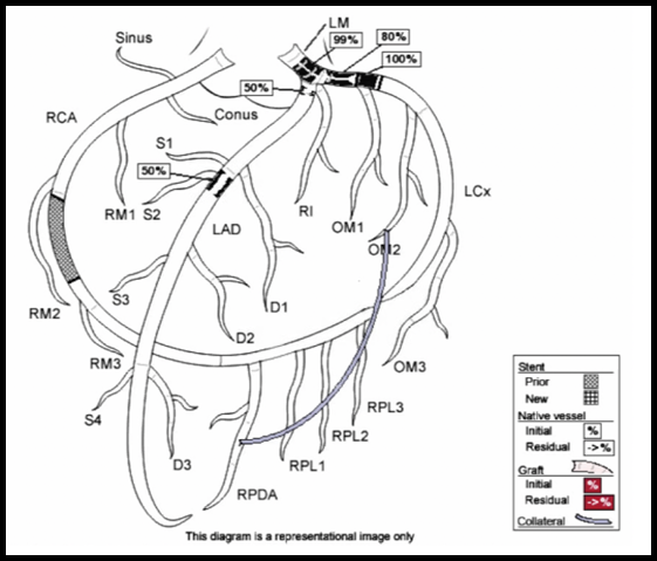
The patient was admitted to the interventional cardiology service. Cardiac catheterization revealed 99% stenosis of the left main coronary artery, 50% stenosis of the left anterior descending coronary artery and 100% occlusion of the previously stented left circumflex. The previously stented right coronary artery was patent.
Results of cardiac catheterization are shown below: Interventions: Due to the extent of stenoses, the patient had an intra-aortic balloon pump placed to reduce myocardial oxygen demand. The next day, he underwent multivessel coronary artery bypass grafting. Socio-economic considerations: This case highlights the importance of dual antiplatelet therapy and smoking cessation in patients with stent placement. It also demonstrates the challenges mental health and socioeconomic factors play in the patients’ ability to adhere to treatment plans. Dr. Littmann’s comments:
There are 4 major types of high-risk acute coronary syndrome (ACS) where the ECG does not show diagnostic ST-segment elevation. These include:
References:
0 Comments
|
AuthorThis blog represents important ECG lessons that the Emergency Medicine Residents from Carolinas Medical Center (Charlotte, NC) rotating through the Cardiology service encounter. Test your knowledge with them! The esteemed educators Dr. Laszlo Littmann and Dr. Michael Gibbs serve as the primary content editors and course directors. Archives
September 2020
CategoriesAll Bradycardia Cardiology ECG Lesson Heart Block Syncope Ventricular Tachycardia Vtach |
LEGAL DISCLAIMER (to make sure that we are all clear about this):The information on this website and podcasts are the opinions of the authors solely.
For Health Care Practitioners: This website and its associated products are provided only for medical education purposes. Although the editors have made every effort to provide the most up-to-date evidence-based medical information, this writing should not necessarily be considered the standard of care and may not reflect individual practices in other geographic locations.
For the Public: This website and its associated products are not intended to be a substitute for professional medical advice, diagnosis, or treatment. Your physician or other qualified health care provider should be contacted with any questions you may have regarding a medical condition. Do not disregard professional medical advice or delay seeking it based on information from this writing. Relying on information provided in this website and podcast is done at your own risk. In the event of a medical emergency, contact your physician or call 9-1-1 immediately.
For Health Care Practitioners: This website and its associated products are provided only for medical education purposes. Although the editors have made every effort to provide the most up-to-date evidence-based medical information, this writing should not necessarily be considered the standard of care and may not reflect individual practices in other geographic locations.
For the Public: This website and its associated products are not intended to be a substitute for professional medical advice, diagnosis, or treatment. Your physician or other qualified health care provider should be contacted with any questions you may have regarding a medical condition. Do not disregard professional medical advice or delay seeking it based on information from this writing. Relying on information provided in this website and podcast is done at your own risk. In the event of a medical emergency, contact your physician or call 9-1-1 immediately.


 RSS Feed
RSS Feed