|
1/14/2020 0 Comments December 2019 ECG LessonThis month’s EKG is brought to you by Dr. Clayton Long. Editors: Drs. Littmann and Gibbs  Clayton Long, MD Clayton Long, MD Case A 67-year-old male with 6-12 month history of recurrent syncope presented to the ED with facial trauma following a syncopal event. The patient experienced multiple prodromal episodes of presyncope in short succession, ultimately culminating in true syncope causing a nasal fracture. He refused additional work-up at the time of injury given his history of extensive previously negative evaluations for syncope. He had received multiple ECGs, nuclear stress testing and echocardiography in the past. The results of his past evaluations were unrevealing, and he was referred to a specialist with no further clarity provided. Within weeks he returned for outpatient surgical repair of his nasal fractures. In the perioperative period he was noted to have AV block on telemetry which self-resolved. He was reportedly symptomatic at the time this rhythm was recognized and was referred for subspecialty Cardiology – Electrophysiology (EP) for evaluation where the following ECGs were obtained. What is your interpretation of the ECGs?
Correct interpretation of the ECGs
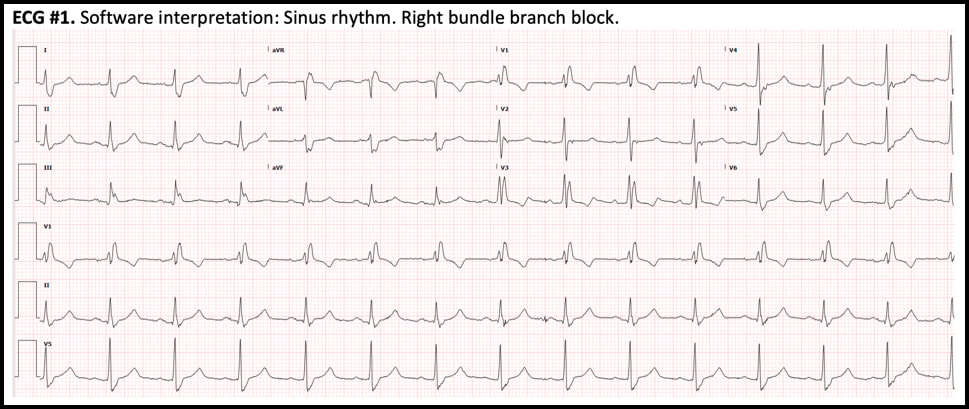
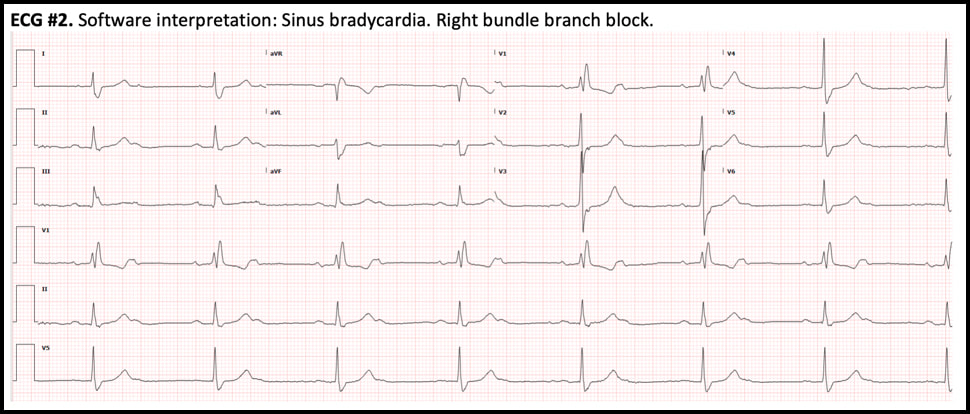
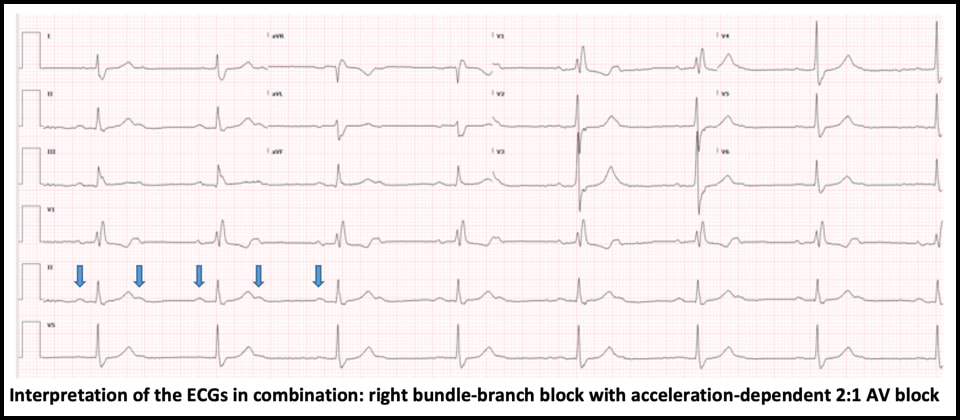
ECG #1 - NSR with normal PR, normal QRS axis and RBBB - Sinus rate of 85/min with 1:1 AV conduction ECG #2 - Regular bradycardia, still normal PR intervals and normal QRS axis, unchanged RBBB pattern - The sinus rate is now 90/min with 2:1 AV block; hence, the ventricular rate is 45/min - Blue arrows below demonstrate twice as many sinus P waves as QRS complexes Significance of these findings?
These ECG findings are consistent with right bundle-branch block and acceleration-dependent second-degree AV block where there is 1:1 AV conduction at slower sinus rates but 2:1 AV block at faster atrial rates. Acceleration- dependent AV block localizes the block to the His-Purkinje system, which is characterized by all-or-none conduction. At a critical sinus rate, only every other sinus impulse is able to conduct through the His-Purkinje system and every other P wave is blocked. On the conducted complexes, there is no change in the PR interval. The blocked P waves are almost never recognized by the interpretation software, which usually reads the rhythm as sinus bradycardia, a clinically trivial dysrhythmia. Therefore, the ECG must be carefully scrutinized in order to identify this ominous rhythm and the correct diagnosis. - In this case, slowing down the sinus rate with carotid massage or IV beta-blocker can paradoxically improve AV conduction. - Atropine, on the other hand, is contraindicated because it can worsen AV conduction by increasing the sinus rate. - This finding is concerning for extensive distal conduction disease. Patients with bundle-branch block and acceleration-dependent AV block are at high risk of complete heart block at an anatomically distal level, which may result in asystole and cardiac arrest. - This finding requires urgent EP evaluation and is an absolute indication for dual-chamber (AV sequential) pacemaker implantation Hospital Course
The patient was admitted directly from the outpatient EP office visit to Cardiology for permanent pacemaker implantation. He received a dual-chamber pacemaker. He continued to experience syncopal symptoms following his initial procedure due to intermittent loss of lead capture requiring revision and a brief admission to the cardiac ICU. The remainder of his hospitalization was uncomplicated, and he was discharged shortly thereafter with no recurrence of symptoms. During his first outpatient EP follow-up he was noted to be asymptomatic with no recurrence of syncope and a fairly low pacing burden. EP noted that they anticipate his pacing burden will increase over time. Summary
This patient had right bundle-branch block and an occult acceleration-dependent 2:1 AV block that was present but unrecognized on the ECGs during multiple prior ED visits for syncope. Bundle-branch block combined with acceleration dependent 2:1 AV block is indicative of extensive distal conduction system disease and requires urgent EP evaluation for pacemaker implantation to avoid degeneration to complete heart block and potentially, cardiac arrest. This rhythm is rarely detected by the interpretation software and will be missed on ECG review unless thoughtfully searched for. Dr. Littmann’s Comments
It is well known that patients with bifascicular block are at risk of developing complete heart block. This is especially true for patients with bifascicular block who experience syncope. It is less appreciated, but still well documented that patients with simple left or right bundle branch block and syncope too, as in the current case, are frequently found to have paroxysmal AV block and asystole.1 Based on these data it is recommended that patients with unexplained syncope who have any type of intraventricular block should undergo prolonged monitoring with an implanted loop recorder (class I recommendation).2 In this case, the patient had numerous previous workups by cardiologists and underwent a number of minimal value testing such as echocardiography and stress testing, but was never offered cardiac monitoring. A second important lesson of the case is that 2:1 heart block is almost never recognized by interpretation softwares and is rarely recognized by providers. Most cases are interpreted as sinus bradycardia, which is usually a more benign dysrhythmia. Whenever a patient’s ECG appears to demonstrate regular sinus bradycardia, please carefully search for twice as many P waves than meets the eye by halving the interval between the conducted P waves. This “trick” only takes a few seconds to do. It is most important to search for 2:1 heart block in patients who have bundle-branch block and in patients who present with presyncope or syncope. Key references
0 Comments
|
AuthorThis blog represents important ECG lessons that the Emergency Medicine Residents from Carolinas Medical Center (Charlotte, NC) rotating through the Cardiology service encounter. Test your knowledge with them! The esteemed educators Dr. Laszlo Littmann and Dr. Michael Gibbs serve as the primary content editors and course directors. Archives
September 2020
CategoriesAll Bradycardia Cardiology ECG Lesson Heart Block Syncope Ventricular Tachycardia Vtach |
LEGAL DISCLAIMER (to make sure that we are all clear about this):The information on this website and podcasts are the opinions of the authors solely.
For Health Care Practitioners: This website and its associated products are provided only for medical education purposes. Although the editors have made every effort to provide the most up-to-date evidence-based medical information, this writing should not necessarily be considered the standard of care and may not reflect individual practices in other geographic locations.
For the Public: This website and its associated products are not intended to be a substitute for professional medical advice, diagnosis, or treatment. Your physician or other qualified health care provider should be contacted with any questions you may have regarding a medical condition. Do not disregard professional medical advice or delay seeking it based on information from this writing. Relying on information provided in this website and podcast is done at your own risk. In the event of a medical emergency, contact your physician or call 9-1-1 immediately.
For Health Care Practitioners: This website and its associated products are provided only for medical education purposes. Although the editors have made every effort to provide the most up-to-date evidence-based medical information, this writing should not necessarily be considered the standard of care and may not reflect individual practices in other geographic locations.
For the Public: This website and its associated products are not intended to be a substitute for professional medical advice, diagnosis, or treatment. Your physician or other qualified health care provider should be contacted with any questions you may have regarding a medical condition. Do not disregard professional medical advice or delay seeking it based on information from this writing. Relying on information provided in this website and podcast is done at your own risk. In the event of a medical emergency, contact your physician or call 9-1-1 immediately.
 RSS Feed
RSS Feed