|
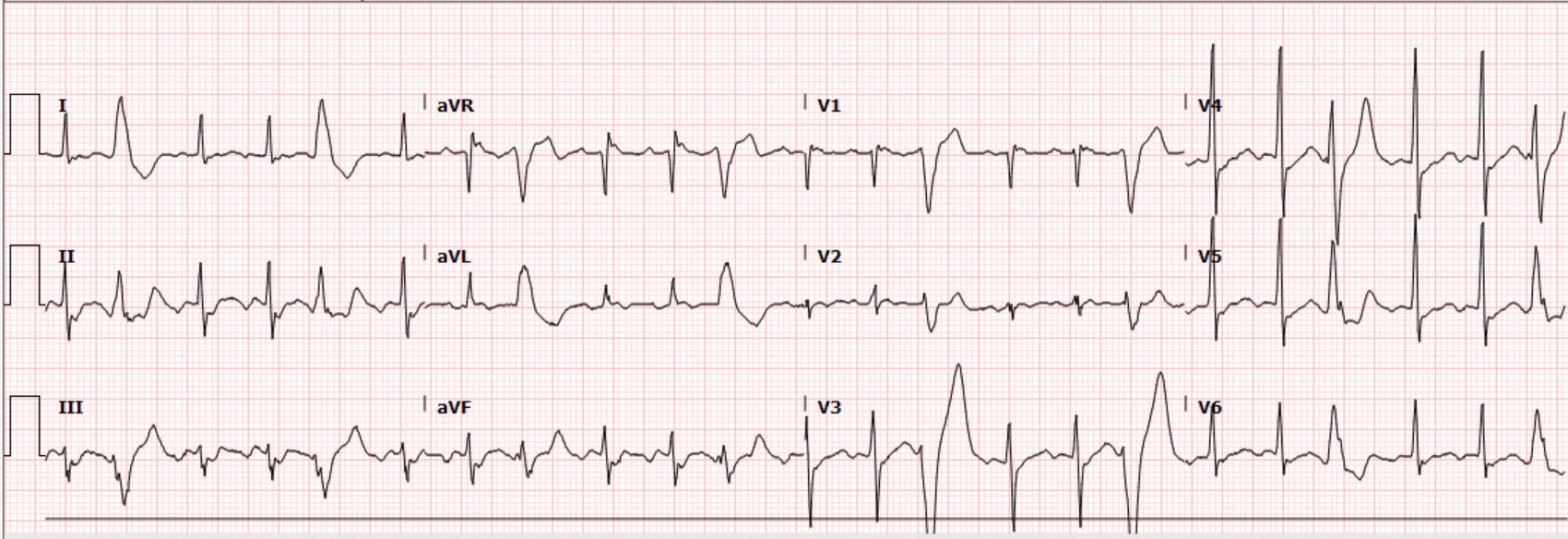
Case: A 63-year-old male with a history of traumatic brain injury and associated seizure disorder presented from a skilled nursing facility after experiencing syncope and recurrent seizures. EMS reported occasional heart rates in the 200s. The patient received 5 mg of midazolam IM and the seizure activity resolved. On evaluation, he appeared to be post-ictal and minimally responsive. He had a normal pupillary exam and was withdrawing all four extremities. He was tachycardic at 136/min, blood pressure 105/75 mmHg, respiratory rate 20/min and oxygen saturation 95% on room air. The following electrocardiogram was obtained: Interpretation by ECG software, confirmed by a physician Sinus tachycardia with frequent premature ventricular complexes What is your interpretation of the ECGs?
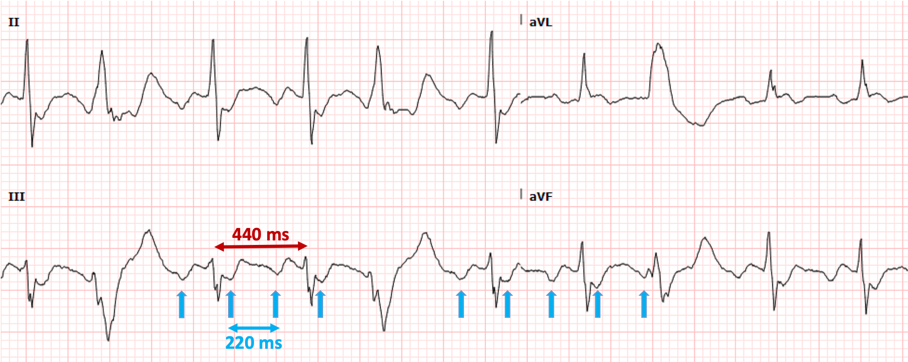
Correct interpretation of the ECG Atrial flutter with 2:1 AV conduction and frequent premature ventricular complexes Summary of key ECG findings:
CLUES:
Clues to recognizing 2:1 flutter include the following simple “tricks”
Significance of finding?
Significance of recognizing 2:1 flutter in cases initially interpreted as sinus tachycardia
HOspital Course
Hospital Course The patient’s pre-hospital report of extreme tachycardia raised the possibility of 1:1 flutter and possibly syncope due to the dysrhythmia rather than seizure. Cardiology evaluated the patient and recognized the atrial flutter. The patient was given IV diltiazem which resulted in excellent rate control. It was felt that because of his brain injury and seizures, the patient was not a candidate for chronic anticoagulation. Catheter ablation was discussed but eventually rejected. Echocardiogram revealed right ventricular dilatation and hypokinesis, moderate tricuspid regurgitation, moderate pulmonary hypertension and marked right atrial dilatation. Dr. Littmann’s Comments
Atrial flutter with 2:1 AV conduction (“2:1 flutter”) is one of the most commonly missed ECG diagnosis, both by the interpretation software and by providers. 2:1 flutter should always be entertained if the computer diagnoses “sinus tachycardia” but there is either an abnormal P-wave morphology and/or an abnormal PR interval. Consistent misreadings by the interpretation software include sinus tachycardia with first-degree AV block, sinus tachycardia with very short PR intervals, and ectopic atrial tachycardia. The most important factor in recognizing 2:1 flutter is to always consider this diagnosis in sick patients who present with a regular SVT. Once the diagnosis of 2:1 flutter is entertained, it is usually easy to prove it by using the “halving method”: recognizing negative P waves in the inferior leads whose distance is exactly half of the R-R intervals. If uncertain, the use of IV adenosine, by exposing the flutter waves, can be very helpful. From the ED physician’s perspective, the most important job is to recognize the flutter and provide rate control. In patients who present repeatedly with atrial flutter, it is also prudent to suggest to the accepting team that curative treatment with catheter ablation should be entertained and discussed with cardiology.
0 Comments
Your comment will be posted after it is approved.
Leave a Reply. |
AuthorThis blog represents important ECG lessons that the Emergency Medicine Residents from Carolinas Medical Center (Charlotte, NC) rotating through the Cardiology service encounter. Test your knowledge with them! The esteemed educators Dr. Laszlo Littmann and Dr. Michael Gibbs serve as the primary content editors and course directors. Archives
September 2020
CategoriesAll Bradycardia Cardiology ECG Lesson Heart Block Syncope Ventricular Tachycardia Vtach |
LEGAL DISCLAIMER (to make sure that we are all clear about this):The information on this website and podcasts are the opinions of the authors solely.
For Health Care Practitioners: This website and its associated products are provided only for medical education purposes. Although the editors have made every effort to provide the most up-to-date evidence-based medical information, this writing should not necessarily be considered the standard of care and may not reflect individual practices in other geographic locations.
For the Public: This website and its associated products are not intended to be a substitute for professional medical advice, diagnosis, or treatment. Your physician or other qualified health care provider should be contacted with any questions you may have regarding a medical condition. Do not disregard professional medical advice or delay seeking it based on information from this writing. Relying on information provided in this website and podcast is done at your own risk. In the event of a medical emergency, contact your physician or call 9-1-1 immediately.
For Health Care Practitioners: This website and its associated products are provided only for medical education purposes. Although the editors have made every effort to provide the most up-to-date evidence-based medical information, this writing should not necessarily be considered the standard of care and may not reflect individual practices in other geographic locations.
For the Public: This website and its associated products are not intended to be a substitute for professional medical advice, diagnosis, or treatment. Your physician or other qualified health care provider should be contacted with any questions you may have regarding a medical condition. Do not disregard professional medical advice or delay seeking it based on information from this writing. Relying on information provided in this website and podcast is done at your own risk. In the event of a medical emergency, contact your physician or call 9-1-1 immediately.

 RSS Feed
RSS Feed