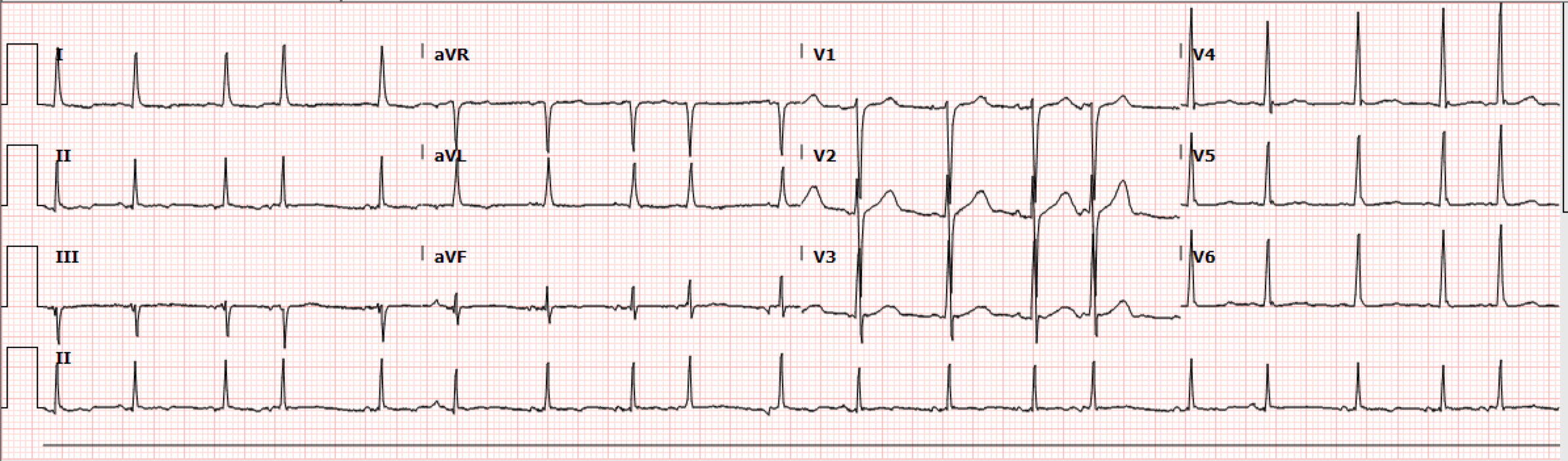
Case:An approximately 70-year-old male with a history of rectal cancer presented to the ED on post-op day five after a lower anterior resection and ileostomy. His hospital course had been uneventful, and he was discharged home on post-op day three. He returned to the hospital, because over the past twenty-four hours he had developed significant abdominal pain, vomiting, and could not tolerate any oral intake. On arrival to the ED he was found to be tachycardic and an EKG was obtained that demonstrated an irregularly irregular rhythm at a rate of about 113 bpm. The patient denied any sensation of racing heart, skipping beats or palpitations. He did not have any history of coronary artery disease or heart failure, but he did endorse a 20 pack-year smoking history. The EKG and Ryhtm Strip are below.CAN YOU IDENTIFY THE RHYTHM?
Diagnosis: Multifocal Atrial Tachycardia Key EKG findings:
What is the Preferred ED Management Strategy?
Adults
Children
MAT itself does not usually require intervention. It is most commonly seen in the elderly population. This rhythm emerges secondary to an underlying pulmonary (most often COPD) and/or cardiac disease. It acts as a poor prognostic indicator in the acutely ill with studies showing up to a 60% in-hospital mortality rate with mean survival of a little over 1 year afterwards. Dedication to treatment in the Emergency Department setting should be focused on the underlying condition. Subsequently, electrolyte repletion should be performed along with pharmacologic management in those showing signs of acute decompensation of their illness or symptomatic persistence of their arrhythmia. Note that cardioversion and class I or class III antiarrhythmics have not been proven to be successful in terminating MAT. Cardioversion may lead to life-threatening arrhythmias and should never be used. Anticoagulation is not necessary, which is different when compared to atrial fibrillation. Much like in adults, the focus for children is on intervention when warranted for acute decompensation of illness. However, early detection followed by pediatric cardiology consult and/or follow-up is crucial as MAT in children may be an early warning sign for the development of impending life-threatening arrhythmias. [1] [2] [3] [4] AddITIONAL BACKGROUND INFO:
Cardiopulmonary disease most often triggers MAT. Other disease processes, including diabetes, chronic renal failure, major surgery, electrolyte disturbances as described above, and certain medications that tend to stimulate adrenergic receptors such as methylxanthines, and digoxin toxicity can also lead to this rhythm. MAT is believed to be caused by triggered activity or abnormal automaticity. A reentry process has been postulated, but not fully proven. The trigger for this rhythm is best explained by the abnormal automaticity theory where, for example, a COPD exacerbation leads to hypoxia with eventual acidosis and increased adrenergic activity of which atrial foci are sensitive to. Pulmonary hypertension and other disease processes that can lead to right atrial enlargement and increased right atrial pressures can also lead to abnormal automaticity. [1] [2] [3] Note that MAT can also be found within the pediatric population. It is most often seen in infants. Usually being secondary to underlying disease processes that lead to right atrial enlargement and increasing pressures such as structural heart disease, syndromic diagnosis, RASopathies, and pulmonary diseases that eventually lead to hypoxia and subsequent adrenergic stimulation. Early detection is important as long-standing tachycardia can lead to tachycardia-induced cardiomyopathy in these children. [4] SUMMARY
● Identify and diagnose MAT using EKG: atrial rate >100 bpm, varying P-R intervals, and ≥ 3 different P waves before every QRS present in the background of an irregularly irregular rhythm ● Treat underlying cardiopulmonary condition(s) (most often COPD in the elderly) to resolve MAT ● Potassium and Magnesium repletion helpful ● Consider pharmacological ventricular rate and ectopic atrial rate control in setting of symptomatic decompensation from underlying illness ● Pediatric cardiology consultation for children ● Beware not to confuse MAT for a-fib and a-flutter as their treatments are different and may lead to adverse outcomes in patients with MAT. ● May be confused with frequent premature atrial contractions and wandering atrial pacemaker which both have rates <100 bpm Dr. Littmann's Lessons to Learn
The vast majority of rapid, irregularly irregular rhythms are atrial fibrillation with rapid ventricular response. However, one should always consider the possibility of MAT. MAT is frequently read as AFib by the interpretation software and, unfortunately, also by providers. In the presented case too, the initial diagnosis was AFib with RVR. If superficial review of the ECG suggests AFib with RVR but you see distinct P waves with isoelectric baseline between the complexes, the rhythm is almost certainly MAT. The most important differences in the treatment of MAT vs. AFib include: (1) You should never attempt cardioversion for MAT. Think of MAT as sinus tachycardia with frequent multifocal PACs with variable PR intervals (we just say MAT because it’s easier and faster), and sinus tachycardia is not a shockable rhythm. (2) You should not use digoxin for rate control as it can actually increase the ectopic atrial activity. (3) Anticoagulation is not indicated. Why? Because MAT is sinus tachycardia with multifocal PACs. Beta blockers, diltiazem and verapamil can be given for both conditions but in AFib they are used to control the ventricular response whereas in MAT, these agents can actually suppress the ectopic atrial activity. REFERENCES:
0 Comments
Your comment will be posted after it is approved.
Leave a Reply. |
AuthorThis blog represents important ECG lessons that the Emergency Medicine Residents from Carolinas Medical Center (Charlotte, NC) rotating through the Cardiology service encounter. Test your knowledge with them! The esteemed educators Dr. Laszlo Littmann and Dr. Michael Gibbs serve as the primary content editors and course directors. Archives
September 2020
CategoriesAll Bradycardia Cardiology ECG Lesson Heart Block Syncope Ventricular Tachycardia Vtach |
LEGAL DISCLAIMER (to make sure that we are all clear about this):The information on this website and podcasts are the opinions of the authors solely.
For Health Care Practitioners: This website and its associated products are provided only for medical education purposes. Although the editors have made every effort to provide the most up-to-date evidence-based medical information, this writing should not necessarily be considered the standard of care and may not reflect individual practices in other geographic locations.
For the Public: This website and its associated products are not intended to be a substitute for professional medical advice, diagnosis, or treatment. Your physician or other qualified health care provider should be contacted with any questions you may have regarding a medical condition. Do not disregard professional medical advice or delay seeking it based on information from this writing. Relying on information provided in this website and podcast is done at your own risk. In the event of a medical emergency, contact your physician or call 9-1-1 immediately.
For Health Care Practitioners: This website and its associated products are provided only for medical education purposes. Although the editors have made every effort to provide the most up-to-date evidence-based medical information, this writing should not necessarily be considered the standard of care and may not reflect individual practices in other geographic locations.
For the Public: This website and its associated products are not intended to be a substitute for professional medical advice, diagnosis, or treatment. Your physician or other qualified health care provider should be contacted with any questions you may have regarding a medical condition. Do not disregard professional medical advice or delay seeking it based on information from this writing. Relying on information provided in this website and podcast is done at your own risk. In the event of a medical emergency, contact your physician or call 9-1-1 immediately.


 RSS Feed
RSS Feed