|
Sudden cardiac death = most frequent medical cause of sudden death in athletes
Jason Collier, 28 (2005), basketball Eddie Guerrero, 38 (2005), wrestling Fab Melo, 26 (2017), basketball What is an “athlete?”
When estimating SCD incidence, the population of athletes “at risk” may be difficult to quantify Definition?
These inconsistencies help account for the wide range of estimated incidence of SCD in athletes in prior reports, from 1 in 3,000 up to 1 in 1 million Risk among male Division 1 basketball players = 10x that in the overall athlete population
Causes
The Young Athlete
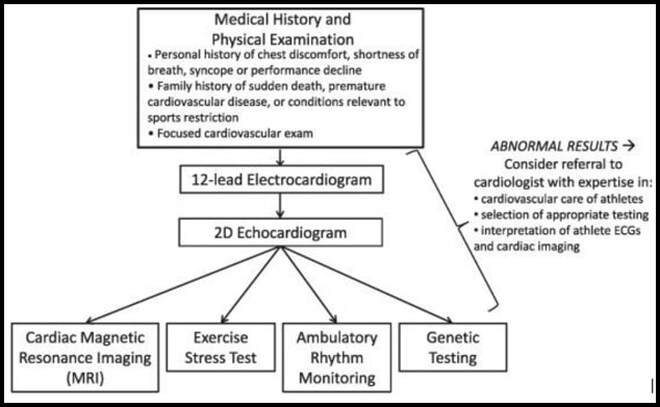
SCD Prevention: Athlete Screening and Evaluation The American Heart Association (AHA) and American College of Cardiology (ACC) recommend screening that is limited to a targeted medical history and physical exam In contrast to the American recommendations, the European Society of Cardiology (ESC) and International Olympic Committee (IOC) advocate for screening that also includes a resting 12-lead electrocardiogram (ECG)
Anatomic/Physiologic Changes
SUMMARY: Although rare, SCD in the athlete is a traumatic event that has a large impact on society Incidence of SCD varies widely depending on the athlete population
All preparticipation screening programs aimed at identifying athletes at high risk of SCD begin with a focused history and physical. The addition of the 12-lead ECG and/or additional cardiac testing is a source of considerable ongoing debate. It is highly unlikely that any screening program will be effective at appropriately identifying all athletes at risk of SCD; therefore, increased access to automated external defibrillators as well as training in cardiopulmonary resuscitation at a community level are important means of reducing SCD in athletes.
0 Comments
11/19/2018 0 Comments Exertion Heat-related Illness
Heat Exhaustion
Heat Stroke
10/26/2018 0 Comments LisFranc Fracture
Introduction
Mechanism & Pathoanatomy
Anatomy
Physical Exam
Imaging
Treatment
10/25/2018 0 Comments Patellar Dislocation
Background
Clinical Features
Evaluation
Management
Disposition
9/21/2018 0 Comments Knee Dislocations
Introduction
Signs & Symptoms
Classification
Diagnostics:
Treatment:
9/14/2018 0 Comments Clavicle Fracture
Background
Clinical Features
Evaluation
Classification
Management
Disposition
9/14/2018 0 Comments BiCeps Tendon Rupture
Incidence
Evaluation
9/7/2018 0 Comments Achilles Tendon Injury
Background:
Dx:
Tx:
9/7/2018 0 Comments Mallet FInger Injury
Background:
PE:
Dx:
Tx:
Aluminum and Foam strips Advantages:
Stax Splint Advantages:
Oval-8® Finger Splint Advantages:
|
Archives
May 2019
Categories |
LEGAL DISCLAIMER (to make sure that we are all clear about this):The information on this website and podcasts are the opinions of the authors solely.
For Health Care Practitioners: This website and its associated products are provided only for medical education purposes. Although the editors have made every effort to provide the most up-to-date evidence-based medical information, this writing should not necessarily be considered the standard of care and may not reflect individual practices in other geographic locations.
For the Public: This website and its associated products are not intended to be a substitute for professional medical advice, diagnosis, or treatment. Your physician or other qualified health care provider should be contacted with any questions you may have regarding a medical condition. Do not disregard professional medical advice or delay seeking it based on information from this writing. Relying on information provided in this website and podcast is done at your own risk. In the event of a medical emergency, contact your physician or call 9-1-1 immediately.
For Health Care Practitioners: This website and its associated products are provided only for medical education purposes. Although the editors have made every effort to provide the most up-to-date evidence-based medical information, this writing should not necessarily be considered the standard of care and may not reflect individual practices in other geographic locations.
For the Public: This website and its associated products are not intended to be a substitute for professional medical advice, diagnosis, or treatment. Your physician or other qualified health care provider should be contacted with any questions you may have regarding a medical condition. Do not disregard professional medical advice or delay seeking it based on information from this writing. Relying on information provided in this website and podcast is done at your own risk. In the event of a medical emergency, contact your physician or call 9-1-1 immediately.
 RSS Feed
RSS Feed