|
2/8/2019 0 Comments Vasopressors in the ED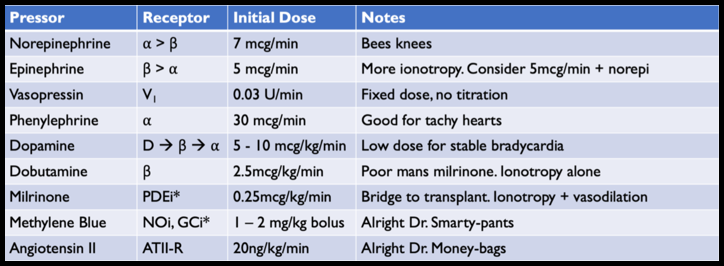
ED Vasopressors – Core Concepts
Our body has 3 major classes of vasopressors - Catecholamines - ⍺/β receptor agonism - Vasopressin – Vasopressor receptor (V1) agonism - Angiotensin II – Angiotensin II Receptor (ATII-R) agonism We use vasopressors to supplement our bodies own mechanisms to increase blood pressure. VASOPRESSOR AGENTS Norepinephrine ONE LINER: THE “BEES KNEES” OF VASOPRESSORS - Mechanism: ⍺/β agonism - Dose: Initial dose 5mcg/min (0.05mcg/kg/min) - Indication: Any shock, the best agent in (ALMOST) all circumstances: SOAP II (NEJM 2010) – Norepi vs dopamine for shock (primarily sepsis); Levy et al (JACC 2018) – Norepi vs epi for post AMI cardiogenic shock; VASST (NEJM 2008) – More norepi vs norepi + vasopressin - Good/bad: (+) Literally the best, (+) Safe for peripheral administration, (-) Can cause arrhythmias Epinephrine ONE LINER: NOT AS GOOD AS NOREPI, MAY HELP A DYING HEART - Mechanism: β/⍺ agonism - Dose: Initial dose 5mcg/min (0.05mcg/kg/min) - Indication: Hypotension + bad heart – hypotension AND bradycardia; hypotension with poor contractility (titrate epi for heart function on POCUS + titrate norepi for BP); Periarrest phase (push-dose epi) - Good/bad: (+) Give a dying heart a better chance (maybe); (+) Can be used in push dose; (-) Lactate no longer reliable for monitoring shock; (-) Increased arrhythmias; (-) Limited evidence that epi is superior to norepi in most situations Phenylephrine ONE LINER: USE FOR IATROGENIC HYPOTENSION OR FOR A FAST HEART - Mechanism: Pure ⍺ - Dose: Initial dose 50mcg/min (0.5mcg/kg/min) - Indication: Sedation induced hypotension, hypotension with arrhythmia (Afib with RVR) - Good/bad: (+) Not arrhythmogenic; (-) Bad in heart failure Dopamine: ONE LINER: POOR MAN’S NOREPI - Mechanism: Dopa/β/⍺ agonism - Dose: Dose dependent effects o Low Doses: 2 – 5 mcg/kg/minàDopa agonismo Mid Doses: 5 – 10 mcg/kg/minàβ agonism o High Doses: 10 – 20 mcg/kg/minà⍺ agonism - Indication: Bradycardia OR Hypotension. If both, use epi - Good/Bad: (-) Arrhythmias; (-) More adverse events compared to norepi Vasopressin: ONE LINER: SUPPLEMENTAL VASOPRESSOR, NEVER AS A SINGLE AGENT - Mechanism: Vasoconstriction via Vasopressin (V1) receptor - Dose: Fixed dose 0.03U/min, no titration. Can use 20U as single bolus in cardiac arrest with steroids (VSE 2013) - Indication: Shock (septic, vasodilatory), renal failure - Good/bad: (+) No adrenergic activity – no arrhythmias, does not compete with catecholamines (+) Maybe decrease need for dialysis compared to norepi (VANISH Trial). (-) No mortality benefit compared to Norepi THE OTHER AGENTS: Almost never used in ED Dobutamine: - Mechanism: β agonism, no ⍺ - Indications: Bradycardia, cardiogenic shock - Dosage: Start at 2.5 mcg/kg/min (Max 20mcg/kg/min) - Notes: Poor-mans milrinone. (-) Bad dysrhythmias. (+/-) Not a true “pressor”; Can cause vasodilation via β2 without ⍺ activity Milrinone: - Mechanism: PDE inhibitor o Increased [Ca]i via cAMPàIonotropy + vasodilation o Lusitropiceffects–Increaseddiastolicrelaxation/filling o IncreasedPreload+Increasedcontractility+decreasedSVR=IncreasedCO - Indications: Heart failure (with goals of transition to either transplant or assist device) - Dosage: 0.25 – 0.5 mcg/kg/min - Notes: (-) Causes arrhythmias. (+/-) Vasodilator. Needs continuous infusion through PICC Methylene Blue: - Mechanism: Inhibit NO/cGMP vasodilation - Indications: Refractory vasodilatory shock - Dosage: 1-2mg/kg as bolus over 15min; Infusion 0.5mg/kg/hr x 4hrs - Notes: Used for refractory hypotension, used for salvage therapy Angiotensin II - Mechanism: Binds Angiotensin-II receptors for direct vasoconstriction - Indications: Refractory vasodilatory shock - Dose: Start at 20ng/kg/min (Max 200ng/kg/min) - Notes: Hasn’t been looked at as solo vasopressor, just for refractory shock with other agents. - Very expensive without mortality benefit (ATHOS-3)
0 Comments
1/4/2019 0 Comments LVAds in your ED
LVAD evaluation in your ED - Think of "LVAD."
Look & Listen Ventricles Anticoagulation Drive Line 10/19/2018 0 Comments Procedural Sedation
Although procedural sedation is a bread and butter component of emergency medicine, it is an area where we can introduce significant harm to our patients. Preparation and being facile with all components of the process if key to doing this safely and efficiently.
Level of Sedation
Prepare for Complications
Know Your Patient
Choose Your Agent
During and Post Procedure
9/26/2018 0 Comments Lupus in your ED
Background:
Understanding Lupus – The Big Picture:
Organ specific problems: Cardiac
Organ specific problems: Respiratory
Organ specific problems: Neuro
Organ specific problems: Vasculitis – resuscitate and give 1g methylprednisone, and suggest to the admitted team they should consider IVIG and/or plasmapheresis!
Organ specific problems: Many others random presentations – if someone has Lupus and a weird problem it can likely be attributed to Lupus, but rule out other causes first. 9/3/2018 0 Comments Nasotracheal Intubation
Nasotracheal Intubation – Core Concepts
As with every sick patient – put on monitors, establish IV access, place on supplemental oxygen. Consider calling for physician backup including another ED provider, anesthesia, or even surgery if available to assist with procedure and possible transition to surgical airway
|
LEGAL DISCLAIMER (to make sure that we are all clear about this):The information on this website and podcasts are the opinions of the authors solely.
For Health Care Practitioners: This website and its associated products are provided only for medical education purposes. Although the editors have made every effort to provide the most up-to-date evidence-based medical information, this writing should not necessarily be considered the standard of care and may not reflect individual practices in other geographic locations.
For the Public: This website and its associated products are not intended to be a substitute for professional medical advice, diagnosis, or treatment. Your physician or other qualified health care provider should be contacted with any questions you may have regarding a medical condition. Do not disregard professional medical advice or delay seeking it based on information from this writing. Relying on information provided in this website and podcast is done at your own risk. In the event of a medical emergency, contact your physician or call 9-1-1 immediately.
For Health Care Practitioners: This website and its associated products are provided only for medical education purposes. Although the editors have made every effort to provide the most up-to-date evidence-based medical information, this writing should not necessarily be considered the standard of care and may not reflect individual practices in other geographic locations.
For the Public: This website and its associated products are not intended to be a substitute for professional medical advice, diagnosis, or treatment. Your physician or other qualified health care provider should be contacted with any questions you may have regarding a medical condition. Do not disregard professional medical advice or delay seeking it based on information from this writing. Relying on information provided in this website and podcast is done at your own risk. In the event of a medical emergency, contact your physician or call 9-1-1 immediately.
 RSS Feed
RSS Feed