|
8/16/2018 0 Comments Pain Management in Our ED
Sergey Motov, MD
@painfreeED General Principles:
0 Comments
8/5/2018 0 Comments Hyperemesis Gravidarum
Hyperemesis Gravidarum:
8/2/2018 0 Comments Pediatric Nasal Foreign Bodies
Background:
7/14/2018 0 Comments Upper GI Bleeds
Stable UGIB
DDx:
Treatment:
Disposition: Risk scoring systems to help risk stratify
Unstable UGIB
Core Concepts:
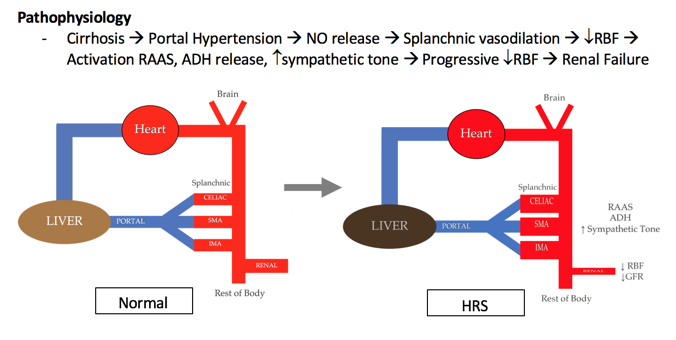
7/3/2018 0 Comments Hepatorenal Syndrome
Hepatorenal Syndrome: Core Concepts
Hepatorenal Syndrome (HRS) = Liver Disease + Acute Kidney Injury (AKI)
Treatment
Management in the ED
5/6/2018 0 Comments Acute Urinary RetentionAcute Urinary Retention Slides by Dr. Covell below:4/12/2018 0 Comments The Dying Asthma PatientOutline The Dying Asthmatic Patient:
3/25/2018 0 Comments INcreased ICP
Increased Intracranial Pressure
Russell Trigonis PGY-2, Katie Lupez PGY-2, and Chris Gardner PGY-1
3/11/2018 0 Comments MEthylene Blue use in the EDMethylene Blue Summary
|
LEGAL DISCLAIMER (to make sure that we are all clear about this):The information on this website and podcasts are the opinions of the authors solely.
For Health Care Practitioners: This website and its associated products are provided only for medical education purposes. Although the editors have made every effort to provide the most up-to-date evidence-based medical information, this writing should not necessarily be considered the standard of care and may not reflect individual practices in other geographic locations.
For the Public: This website and its associated products are not intended to be a substitute for professional medical advice, diagnosis, or treatment. Your physician or other qualified health care provider should be contacted with any questions you may have regarding a medical condition. Do not disregard professional medical advice or delay seeking it based on information from this writing. Relying on information provided in this website and podcast is done at your own risk. In the event of a medical emergency, contact your physician or call 9-1-1 immediately.
For Health Care Practitioners: This website and its associated products are provided only for medical education purposes. Although the editors have made every effort to provide the most up-to-date evidence-based medical information, this writing should not necessarily be considered the standard of care and may not reflect individual practices in other geographic locations.
For the Public: This website and its associated products are not intended to be a substitute for professional medical advice, diagnosis, or treatment. Your physician or other qualified health care provider should be contacted with any questions you may have regarding a medical condition. Do not disregard professional medical advice or delay seeking it based on information from this writing. Relying on information provided in this website and podcast is done at your own risk. In the event of a medical emergency, contact your physician or call 9-1-1 immediately.
 RSS Feed
RSS Feed